
Nutritional intake for the prevention and management of frailty
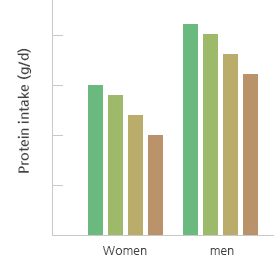
Figure 1. Trend of Protein intake in both men and women as age increased
(National Health and Nutrition Survey)
Korean Frailty and Aging Cohort Study (KFACS)
Kyung Hee University Medical Center, 23 Kyung Hee Dae-ro, Dongdaemun-gu, Seoul 130-872, Republic of Korea.
TEL:02-958-8114 / E-mail:admin@kfacs.kr
COPYRIGHT(C) KFACS ALL RIGHTS RESERVED.